Table of Contents
With aging comes a host of potential medical problems that can reduce a person’s quality of life. Some of these conditions can even eliminate independence and increase morbidity and mortality risks. Osteoporosis is one such condition, with hip fractures resulting in a 20 to 40% mortality rate within one year of the incident. Men have a higher mortality risk than women. Studies show that only 2 out of every 5 patients with hip fractures can return to the level of activity they had before the fracture. For that reason, we look at osteoporosis causes and treatment options.
Osteoporosis is of great concern to many people. While women are more likely to develop osteoporosis, men are at increasing risk as testosterone levels decline. Because men are also less likely to undergo screening for osteoporosis, they often find out they have the condition following a fracture. Estimates show that an osteoporotic fracture occurs every 3 seconds. As many as one in four men and one of every two women may experience a bone fracture related to osteoporosis.
Many issues lead to an increased risk of developing osteoporosis, including hormonal imbalance, medical conditions, certain medications and treatments, and even some lifestyle habits. In this report, we will look at the following while addressing the guidelines and treatment options:
- Definition of osteoporosis
- Symptoms
- Causes
- Prevention
- Hormonal interactions
Osteoporosis occurs as new bone cell production slows down and cannot keep up with the resorption process of old bone cells. Osteoporosis symptoms include height loss, back pain, stooped posture, and bone fractures.
Definition of Osteoporosis
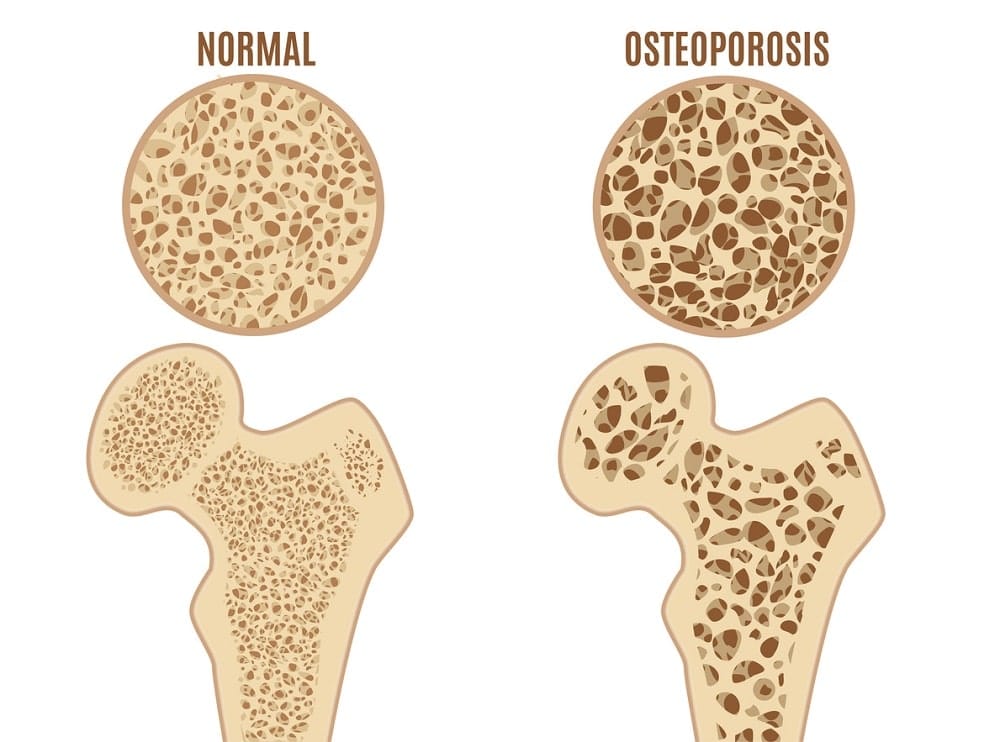
Osteoporosis is a word that means porous bone. At every age, our bones undergo a growth and transformation process. Although we typically reach adult height by age twenty, and that is when we experience peak bone mass, bone is living tissue and continuously undergoing a remodeling process. The entire skeletal structure changes every seven years. As old bone cells die, they are resorbed, and new ones take their place. When there are not enough new bone cells produced daily, the bones become weak and lose their density.
Healthy bones have the appearance of a honeycomb. As bone density decreases, the spaces and holes in the honeycomb structure become larger. The bones become porous, brittle, weaken, and the risk of osteoporosis increases.
Symptoms of Osteoporosis
Understanding and identifying the symptoms of osteoporosis are crucial for adults. Because osteoporosis increases fracture risk, there is also a concern about limited mobility, isolation, and depression. Many adults require long-term care in a nursing home, which puts them at risk of developing other health concerns, including blood clots, infections, and pneumonia. Since we cannot physically see our bones becoming weak, we have to look for other osteoporosis symptoms in hip, spine, and limbs.
What are the symptoms of osteoporosis of the spine, back, and hips?
The symptoms of osteoporosis in upper back often show up as a curvature, with a person giving the appearance that he or she is leaning forward. Another common sign of spine and back bone mineral decline is height shrinkage. The age-old joke of shrinking with age is not funny – it is actually a sign of decreasing bone density. Pain, stiffness, and limited movement in the hips is another concern for osteoporosis.
The most common osteoporosis symptoms include:
- Loss of height
- Stooped posture
- Back pain
- Bone fracture
Some early signs of osteoporosis include:
- Weak and brittle nails
- Receding gums
- Weak grip strength
FAQ
Can osteoporosis cause pain?
Yes, many people with osteoporosis express frequent back pain.
Who is at risk for osteoporosis?
Any adult is at risk of developing osteoporosis. However, specific issues such as ethnicity, gender, age, body frame, illnesses, medications, and lifestyle habits may increase that risk.
How do you diagnose osteoporosis?
To check bone density, the doctor will order a dual-energy X-ray absorptiometry (DEXA) to measure your hips, wrists, or spine. Many doctors will also run comprehensive blood and urine tests to check for underlying medical conditions that can lead to bone loss.
Causes of Osteoporosis
For some adults, the onset of osteoporosis could have started in childhood, if certain medical conditions inhibited bone development. The more bone mass attained in youth, the lower the risk of osteoporosis in adulthood.
What causes osteoporosis?
There is no easy answer to that question. Many varied risk factors exist, some of which are uncontrollable or unchangeable, such as gender, age, family history, body frame, and race. Individuals who are Caucasian or Asian have a greater risk of developing osteoporosis.
Medical conditions that contribute to osteoporosis risks are sometimes preventable, such as dietary choices and lack of exercise that can increase diabetes prevalence or alcohol abuse that can lead to liver disease. Unfortunately, many of the health issues that contribute to osteoporosis are beyond a person’s control.
The following conditions, diseases, and medical procedures increase the risk of bone loss and osteoporosis:
- Autoimmune:
- Ankylosing spondylitis
- Lupus
- Multiple sclerosis
- Rheumatoid arthritis (RA)
- Bone:
- Thalassemia
- Cancer:
- Breast
- Prostate
- Digestive and Gastrointestinal:
- Celiac disease
- Inflammatory bowel disease (IBD – Crohn’s and Colitis)
- Weight loss surgery (bariatric, gastrectomy, gastrointestinal bypass)
- Endocrine:
- Cushing’s syndrome
- Diabetes
- Irregular periods
- Premature menopause
- Thyrotoxicosis
- Hematologic/Blood:
- Leukemia
- Lymphoma
- Multiple myeloma
- Sickle cell disease
- Mental Illness:
- Depression
- Eating disorder
- Nervous System/Neurological:
- Multiple sclerosis (MS)
- Parkinson’s disease
- Spinal cord injuries
- Stroke
- Other Conditions and Diseases:
- Chronic kidney disease
- Chronic obstructive pulmonary disease (COPD)
- Female athlete triad
- HIV/AIDS
- Liver disease
- Oophorectomy – ovarian removal
- Organ transplants
- Polio
- Scoliosis
- Weight loss
- Diet
- Eating disorders
- Low calcium intake
- Poor dietary choices and lack of nutrients
- Reduced protein intake
- Underweight – being underweight can increase bone loss
- Hormones
- Cortisol
- Estrogen
- Growth hormone
- Parathyroid hormone
- Progesterone
- Prolactin
- Testosterone
- Thyroid hormone
- Inactivity
- Lack of exercise
- Sedentary lifestyle
- Sun – lack of sun exposure decreased vitamin D
- Medications
- Antacids containing aluminum
- Antiseizure medications (Dilantin®, Phenobarbital)
- Aromatase inhibitors (Arimidex®, Aromasin®, Femara®)
- Chemotherapy drugs
- Cyclosporine A and FK506 (Tacrolimus)
- Depo-Provera® contraceptive
- Glucocorticoids (cortisone, prednisone)
- Gonadotropin-releasing hormone (Lupron®, Zoladex®)
- Heparin
- Lithium
- Methotrexate
- Proton pump inhibitors (Nexium®, Prevacid®, Prilosec®)
- Selective serotonin reuptake inhibitors (Lexapro®, Prozac®, Zoloft®)
- Tamoxifen® (used for premenopausal symptoms)
- Thiazolidinediones (Actos®, Avandia®)
- Thyroid hormone excess usage
- Smoking and Alcohol
- Alcohol – more than two drinks each day can alter bone remodeling and increase the loss of calcium
- Smoking – tobacco contributes to a weakening of the bones by also blocking how the body uses calcium, estrogen, and vitamin D
One significant concern is when people have used steroid medications for longer than three months to treat conditions such as Crohn’s disease, asthma, rheumatoid arthritis, lupus, and more. Steroids significantly increase bone loss, and it is crucial to increase vitamin D and calcium intake. A person who is using steroids should avoid smoking and get plenty of exercises.
How to Prevent Osteoporosis
You can help reduce the risk of osteoporosis through some lifestyle changes, such as regular exercise, avoiding alcohol and tobacco, and getting enough calcium and vitamin D. A healthy diet plays a significant role in the prevention of osteoporosis as it will also help keep your weight under control. Weight-bearing and resistance training exercises help strengthen the bones.
In addition to vitamin D and calcium, a healthy diet for bones will also include the following:
- Magnesium
- Protein
- Vitamin K
- Zinc
Medications that treat osteoporosis are bisphosphonates, and include:
- Actonel (risedronate)
- Boniva (ibandronate)
- Fosamax (alendronate)
- Prolia (denosumab)
- Reclast (zoledronic acid)
In the next sections, we look at hormones and bone density and how hormone replacement therapy can help strengthen bones.
Hormones and Bone Density
We often think of menopause as a condition that significantly increases the risk of osteoporosis. Not only is that true for women, but andropause or low testosterone is also a leading cause for men. What many females do not realize is that testosterone decline can also weaken their bones. The first five to seven years after the start of menopause can result in a loss of up to 20% of bone density.
How do hormones influence the various types of bone cells?
Hormones control nearly every function in the body. Numerous hormones influence bone cell production, death, and resorption – the cycle of bone remodeling.
Growth hormone (GH) is a leading player in the bone remodeling cycle. First, GH promotes the release of insulin growth factor 1 (IGF-1) by the liver. Next, IGF-1 influences the development of various skeletal cell lineages while GH stimulates the production of osteoblasts and chondrocytes. IGF-1 also mediates the cell regenerating effects of GH. Together, these two hormones promote the production of new bone cells, while IGF-1 also helps stimulate bone resorption. Reduced bone mineral density is commonly seen in patients of all ages who have growth hormone deficiency (GHD).
Osteoblasts need not only growth hormone but also testosterone, which supports both their production and prevents their apoptosis (early death). Osteoclasts are crucial for bone resorption and require estrogen to support that process. Whereas testosterone, estrogen, and growth hormone help support new bone cells, estrogen also reduces bone turnover.
Contrary to popular belief, vitamin D is actually a hormone called calcitriol, which helps the body absorb and use calcium. Lack of vitamin D is a significant factor in osteoporosis. 15 minutes of sunshine each day can help the body produce more vitamin D. Supplements are also available and beneficial for many people.
What Hormonal Imbalance Can Cause Osteoporosis
A variety of hormonal imbalances can increase the risk of osteoporosis, including:
- Low estrogen:
Estrogen deficiency is a leading cause of osteoporosis in women.
- Low testosterone:
Declining testosterone levels can lead to reduced osteoblast differentiation
- Growth hormone deficiency:
Pituitary-produced growth hormone begins to decline before age thirty, reducing the supply of new bone cells
- Hypothyroidism:
Although an underactive thyroid does not increase osteoporosis risk, too much thyroid hormone medication can lead to bone loss
- Hyperthyroidism:
High thyroid hormone levels can increase bone loss
- Hyperparathyroidism:
Causes urinary calcium loss which weakens the bones
- Excess cortisol:
Low growth hormone and testosterone levels are common in people who have high cortisol (stress hormone) levels
Hormone levels can decline due to age, tumors, head or testicular injuries, medications, surgical or radiation treatments, lifestyle factors, and unknown causes. When a hormonal imbalance contributes to increased osteoporosis risk, then treatment with the appropriate hormone therapy can help.
Hormonal Replacement Treatment for Osteoporosis
Treatment with hormone replacement therapy may have some benefits for people dealing with osteoporosis. The first thing to do if you suspect you have osteoporosis is to contact a hormone specialist (endocrinologist) for a complete and comprehensive blood panel screening. Finding out which hormones are out of balance or deficient is the first step in how to treat declining bone mineral density. A person should never begin hormone therapy without first undergoing full diagnostic testing, including a physical examination and review of one’s medical history.
Once the doctor determines the need for hormone replacement treatment, the appropriate medication is then prescribed. Some hormone treatments, such as growth hormone and testosterone, are mutually beneficial. Many people are deficient in both of these hormones and increasing one can often improve the other as they reciprocally boost each other’s production. Additionally, the body naturally converts some of the excess testosterone into estradiol. That means that testosterone therapy can help boost both testosterone and estrogen levels at the same time.
Here are some of the various types of hormone replacement therapy that can help osteoporosis:
- Estrogen Therapy:
Helps preserve bone density by reducing bone turnover – however, estrogen does increase certain other risks for women.
- Estrogen/Progesterone Therapy:
Some menopausal women may receive a combination treatment – however, it is crucial to ask for bioidentical progesterone and not synthetic progestin, which can increase blood clot and cancer risk.
HGH therapy helps strengthen bone density in adults with growth hormone deficiency.
- Progesterone Therapy:
Progesterone may help stimulate osteoblasts but may not work well enough on its own to improve BMD.
Along with improving growth hormone and estrogen levels (through estradiol conversion), testosterone works directly on new bone cells to improve bone density.
Do not undergo hormone replacement therapy without doctor authorization, supervision, and comprehensive blood analysis. For more information on preventing or treating osteoporosis, please contact our hormone clinic for a free, confidential consultation.




No Comments
Sorry, the comment form is closed at this time.