What Is Metabolism and How Does HGH Affect Metabolic Health?
Table of Contents
- What Is Metabolism and Why Is It Important?
- What Are the Most Serious Metabolic Health Issues in 2021?
- The Main Components of a Healthy Metabolism
- How Does Human Growth Hormone (HGH) Affect Metabolism?
- Steps You Can Take Today to Improve Your Metabolic Health for a Lifetime
- The Bottom Line on Optimizing Your Metabolic Health
If you are one of the millions of Americans affected by dysfunctional metabolism, human growth hormone (HGH) has an enormous role to play in restoring your metabolic health for long-term improvements in wellness and a reduced risk of future illness.
With a disturbing rise in diabetes and other metabolic disorders among the US population, healthcare interventions to improve metabolism are needed now more than ever. To protect your health now and into the coming years, here is everything that you should know about metabolism, how HGH affects it, and steps that you can take today to improve your metabolism.
What Is Metabolism and Why Is It Important?
To function, your body requires energy – to generate muscular contraction during exercise, to break down food during digestion, to repair tissues during sleep, and to power the brain and its many complex processes.
Metabolism — in its simplest definition — is the processing, storage, and usage of energy. Through diet, we take in calories (energy) that our bodies need to perform various daily tasks to maintain health. When our metabolism is humming along at full speed, we enjoy high energy levels that last throughout the day while our organs and tissues receive the vital nourishment that they require.
The Negative Health Effects of Poor Metabolism
Dysfunctional metabolism can wreak havoc on health, contributing to or directly causing a variety of negative effects such as:
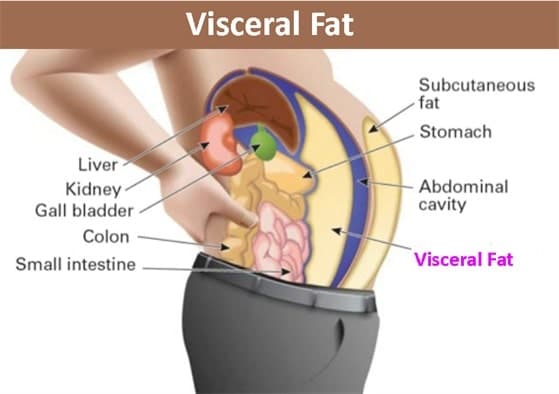
- Unwanted fat buildup (especially visceral fat). Excess energy that we take in through the foods that we eat is stored as fat. Individuals with healthy metabolisms burn more calories, so they don’t store as much fat. On the other hand, slow or dysfunctional metabolisms increase body fat. One of the telltale signs of impaired metabolism is the accumulation of visceral fat around the belly. This is commonly referred to as “belly fat” or a “beer belly.”
- Chronic inflammation. Poor metabolism contributes substantially to the development of chronic, low-grade inflammation. Untreated chronic inflammation, in turn, is a known driver of nearly every form of chronic illness, including cancer, heart disease, and autoimmune disorders.
- Poor energy levels. Because metabolism is the process that your body uses to generate energy for itself, individuals with an abnormally slow or impaired metabolism struggle to maintain their energy throughout the day.
- Dangerous cholesterol levels. Poor metabolism affects cholesterol levels in two critical ways: by lowering HDL (the beneficial type of cholesterol that you need to maintain healthy blood vessels) while simultaneously increasing triglyceride levels, an undesirable form of lipid (fat) that increases the risk of serious cardiovascular events such as heart attack.
- Depression. Major depressive disorder (MDD), the most common type of depression, affects 16 million adults. Researchers have begun in recent years to better identify the mechanisms that underlie the known link between metabolic dysfunction and depression.
What Are the Most Serious Metabolic Health Issues in 2021?
Let’s take a look at the most serious metabolic health issues affecting US patients in 2021.
Diabetes
Of all metabolic disorders, diabetes mellitus (DM) (often referred to as just “diabetes”) is the most well-known – likely due to its alarming and growing prevalence among the US population. According to data from the US Centers for Disease Control (CDC), 34 million Americans have diabetes.
Two forms of diabetes have different causes and treatments:
- Type 1 diabetes. Patients with type 1 diabetes are unable to produce insulin (needed for food processing) in the pancreas where the hormone is normally manufactured. As a result, blood sugar management becomes impossible. Type 1 diabetes is most commonly attributed to an inherited genetic condition in which the body generates an autoimmune response that targets pancreatic cells, although the precise cause of this form of diabetes remains unclear.
- Type 2 diabetes. As opposed to type 1 diabetes in which the pancreas doesn’t produce insulin, the pancreas in individuals with type 2 diabetes does produce insulin. The underlying issue in type 2 diabetes is a lack of response to insulin, which normally triggers cells to take in sugar in the blood for energy. In type 2 diabetics, the cells don’t respond appropriately to signals from insulin, so sugar remains in circulation in the blood, often at dangerous levels.
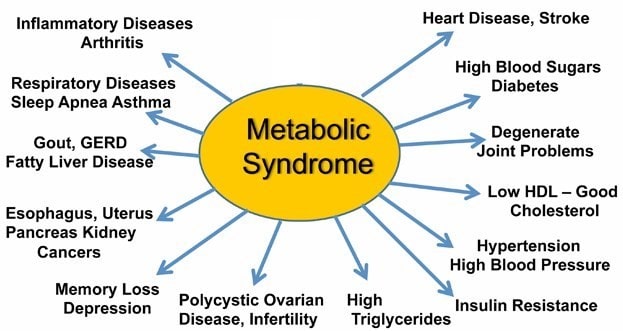
Metabolic Syndrome
Although diabetes gets more public attention, metabolic syndrome is more common: 33% of Americans exhibit the clinical signs of metabolic syndrome. The diagnostic criteria for metabolic syndrome differ from those for most diseases. Rather than representing a single disorder, metabolic syndrome is a cluster of five interrelated markers:
- Excessive belly fat (determined by a waistline over 40 inches in men or 35 inches in women)
- High blood pressure
- High fasting blood sugar (due to insulin resistance)
- Elevated triglycerides
- Low levels of high-density lipoprotein (HDL) – the healthy cholesterol
Critically, metabolic syndrome can cause or worsen a wide array of negative health conditions, as illustrated in the graphic below. Several risk factors increase an individual’s chances of developing metabolic syndrome. These are:
- Smoking. The evidence shows that metabolic syndrome is more common in smokers than in non-smokers.
- Age. Risk increases across time, with seniors having the greatest vulnerability.
- Obesity. Higher fat accumulation (especially visceral fat around the belly) impairs metabolic function.
- Diabetes. Insulin resistance is a common feature of metabolic syndrome.
- Sleep apnea.
Less Common Metabolic Disorders
In addition to diabetes and metabolic syndrome, a number of other rare conditions can also impair proper metabolic function. Examples include:
- Gaucher’s disease
- Hereditary hemochromatosis
- Glucose galactose malabsorption
- Phenylketonuria (PKU)
‘Healthy Obesity’ vs ‘Unhealthy Obesity’: What Is the Difference?
Although obesity is closely linked to poor metabolism, not everyone who is obese suffers from a metabolic disorder. One of the more nuanced aspects of assessing metabolic health, therefore, is the clinical distinction between so-called “healthy obesity” vs “unhealthy obesity.” First, it’s important to understand the metrics that healthcare providers use to determine a diagnosis of obesity. Most doctors use a scale called the body mass index (BMI). This is the formula:
BMI = kg/m2
To arrive at your own BMI, simply convert your weight to kilograms from pounds (if you are American) and your height from feet and inches to meters. Then divide your weight in kilograms by your height in meters squared. The web is full of free BMI calculators that anyone can use as a DIY healthcare resource.
Your BMI will correspond to one of the categories in the BMI scale.
| BMI Scale | |
| BMI Score | Health Status |
| <18.5 | Underweight |
| 18.5-24.9 | Healthy weight |
| 25.0-29.9 | Overweight |
| 30.0-34.9 | Obesity class 1 |
| 35-39.9 | Obesity class 2 |
| >40 | Obesity class 3 |
The term “metabolically healthy obese” (MHO) refers to cases in which the patient qualifies clinically as obese (as measured by a BMI above 30) but he or she does not present with any signs of impaired metabolism or related conditions.
For example, one study examining the cardiovascular health of MHO vs metabolically unhealthy subjects found that “subclinical impairment of myocardial function is more closely associated with adverse metabolic health than with either obesity or BMI.”
These findings show that optimizing your metabolic health, potentially, is more important for preventing disease and maintaining wellness than a stand-alone measurement of body fat. But how do you know if you are metabolically healthy or unhealthy?
How Do You Know if You Are Metabolically Healthy or Unhealthy?
Unfortunately, “there is currently no consensus on how to define metabolic health or metabolically healthy obesity except for the inclusion of obesity.”
However, the best indicator of metabolic health currently available is a combination of lab tests – called a Comprehensive Metabolic Panel (CMP) — that can paint an overall picture of how your body processes, uses, and stores energy:
- Glucose (the form of sugar the body predominately uses for energy)
- Electrolytes (sodium, potassium, magnesium, and chloride)
- Calcium
- Albumin
- Total protein
- Alkaline Phosphatase (ALP), Alanine Transaminase (ALT), and Aspartate Aminotransferase (AST)
- Bilirubin
- Creatinine
- Blood urea nitrogen (BUN)
These various markers indicate how efficiently your body takes in and distributes energy and eliminates the waste products that result.
The Main Components of a Healthy Metabolism
Below, we will explore the main components of a healthy metabolism, starting with perhaps the most fundamental factor at play, blood sugar, followed by triglycerides, HDL cholesterol, and blood pressure.
Blood Sugar
An inability to properly metabolize blood sugar (glucose) is one of the telltale signs of metabolic dysfunction. Individuals whose insulin hormones cannot shuttle enough circulating blood sugar into the cells where it is normally deposited experience a clinical condition called “insulin resistance.” Some public health groups estimate that as many as 1/3 of all Americans suffer from some degree of insulin resistance.
Left unchecked, insulin resistance will develop into diabetes. A diagnosis of “pre-diabetes” means that blood sugar levels are elevated but not yet high enough to indicate full-blown diabetes.
| Blood Sugar Levels Chart | |||
| Before Eating (Fasting) | Immediately After Eating | 3+ Hours After Eating | |
| Normal | 80-100 | 170-200 | 120-140 |
| Pre-Diabetic | 101-125 | 190-230 | 140-160 |
| Diabetic | 126+ | 220-300 | 200+ |
Ideally, the best time to test your blood sugar is while you are fasting because testing levels during this time offers the most accurate picture of your current metabolic function. For this reason, many doctors recommend that their patients perform blood sugar testing in the morning before they have eaten.
The factors that often contribute to elevated fasting blood sugar levels are:
- Lack of exercise
- Constant eating (“grazing”) throughout the day
- Stress
- Acute illness (i.e., an infection like the flu)
Triglycerides
Although they are commonly referred to as a form of cholesterol next to LDL and HDL cholesterol, triglycerides are not technically cholesterol. Rather, they are fatty deposits that store energy for later use.
Triglycerides are dangerous at high concentrations in the blood because they drive atherosclerosis, the age-related hardening of the arteries that constricts blood flow and, over time, increases the risk of heart attack and stroke significantly.
| Triglyceride Reference Chart | |||
| Normal | Borderline High | High | Extremely High |
| <1.7 | 1.7-2.1 | 2.2-5.4 | >5.5 |
*As measured by millimoles per liter (mmol/L.)
High triglyceride levels can be caused by:
- Poor diet, especially ones heavy in processed foods.
- Lack of regular exercise.
- Excessive alcohol consumption.
- The use of certain medications such as beta blockers, immunosuppressants, and steroids
- Genetic disorders that disrupt the efficient conversion of fat to energy
- Low thyroid hormones (T3 and T4)
High-Density Lipoprotein (HDL Cholesterol)
Despite the popular perception that all cholesterol is unhealthy, HDL cholesterol is actually beneficial and enormously important for keeping blood flowing unobstructed through the cardiovascular system.
One handy way to remember the important distinction between HDL (which you want more of) and LDL (the harmful type) is that LDL “lays down” the fatty deposits in the blood vessels while HDL “hauls it away” to be processed by the liver. In this way, HDL keeps the arteries open and clog-free.
The difference in function between HDL and LDL is the reason that a raw, or “total,” cholesterol count can be misleading. Instead, the ratio of HDL to LDL is a much more important marker of metabolic health; the goal of any cholesterol management plan is to elevate HDL levels while decreasing LDL levels.
HDL cholesterol is actually beneficial and enormously important for keeping blood flowing unobstructed through the cardiovascular system.
The American Heart Association (AHA) recommends an optimal ratio of 3.5:1 in terms of total cholesterol counts compared to HDL counts. So, for example, if your total cholesterol count is 150, then you should strive for an HDL count of about 42.
Any HDL-to-total cholesterol ratio above 5 for men or 4.4 for women indicates a heightened risk of heart disease and other complications.
Clinically low HDL are often attributable to:
- Obesity
- Smoking
- Lack of regular exercise
- Medications like beta blockers
- Diet high in refined carbohydrates (sugar, white bread)
Blood Pressure
Blood pressure is a measurement of how strenuously the heart must pump to deliver an adequate supply of oxygen and nutrients to the organs and tissues that need them. Blood pressure is measured in two ways: diastolic and systolic pressure. Diastolic pressure refers to the amount of pressure inside the arteries as they deliver blood from the heart throughout the body. Systolic pressure measures the pressure applied to the artery walls during each heartbeat. Both numbers are important to keep in the green range above to maintain your health.
The following lifestyle and physiological factors can drive high blood pressure:
- Smoking
- Obesity
- A diet high in sodium
- Genetic predisposition
- Age
- High stress levels
The Bottom Line on the Markers of Metabolic Health
As you might have noticed, many of the markers of metabolic health discussed here are interrelated and interdependent – for example, excess triglyceride or LDL cholesterol levels can force the heart muscle to increase the pressure of its contraction, which can further worsen the health threat that those high cholesterol levels pose.
In another example, obesity may make getting regular exercise more uncomfortable or difficult, which can discourage greater activity levels, in turn contributing to a worsening of the markers of poor metabolic health above like high blood sugar.
In effect, poor metabolic health can become a vicious spiral in which the ill health effects converge and multiply. The only way to reverse the trend is a massive lifestyle reorientation (see later section on steps you can take to begin to reverse your metabolic health today).

How Does Human Growth Hormone (HGH) Affect Metabolism?
A small pea-sized structure in the mid-region of the brain called the pituitary gland produces human growth hormone (HGH). As an anabolic (pro-growth) hormone, HGH is responsible for the following functions in the body:
- Maintaining healthy muscle tissue
- Fortifying bone strength/density
- Increasing sexual libido
- Preventing mental health conditions like depression and anxiety
- Regulating body composition (fat distribution)
- Optimizing metabolism for high energy levels and maximum fat burning
Growth Hormone Deficiency and Metabolic Dysfunction
Growth hormone deficiency (GHD), also called “hypopituitarism,” is a condition in which the pituitary gland does not produce enough HGH to sustain good health. Over time, HGH levels tend to drop. As we will explore in the following section, HGH is critical for good metabolic function. Accordingly, low HGH levels can negatively affect metabolism.
How HGH Sustains a Healthy Metabolism
HGH, when it is found in adequate amounts in the blood, sustains healthy metabolism in the following ways:
- Greater protein anabolism (protein synthesis) – the building block of muscle fiber
- Increased amino acid uptake
- Lowered urea levels produced by the kidneys
- Increased fat burning (lipolysis)
- Normalized insulin levels via insulin-like growth factor 1 (IGF-1)
- Reduced belly fat.
An accessible and affordable GH stimulation or GH suppression test can determine whether your pituitary gland produces enough HGH to keep your metabolism running at full throttle.
Steps You Can Take Today to Improve Your Metabolic Health for a Lifetime
Dr. Chih-Hao Lee of the Harvard School of Public Health offers encouragement to anyone hoping to reverse course, improve their metabolism, and reap the health benefits that result; “you can manipulate your metabolism to a degree. It is often a small change that may help you.”
- Exercise regularly. Plenty of exercise is beneficial for nearly every facet of health, including revving up your metabolism. If you are not engaging in at least a moderate form of exercise daily (such as walking), you are depriving your body of the natural benefits of movement – getting your heart pumping, converting stored fat to energy, and optimizing the function of the digestive system. To get the most metabolic advantage from exercise, consider high-intensity interval training (HIIT), weightlifting, or another form of exercise that requires short bursts of maximum output punctuated by short periods of rest.
- Drink green tea. The majority of green tea’s unique health-promoting properties, including the support that it lends for a healthier metabolism, come from a powerful compound called epigallocatechin gallate (EGCG). EGCG acts at the cellular level to prevent the formation of fat, keeps insulin resistance in check, and regulates cholesterol levels. Consider swapping out your morning cup of coffee for green tea.
- Hormone replacement therapy (HRT). HRT is an increasingly common and affordable treatment modality that has achieved near-miraculous health turnarounds in the individuals who receive it, including patients who present with signs of poor metabolism. Ask your doctor how replacement therapy with HGH can help you recover your good health.
- Intermittent fasting (IF). If you are not familiar with intermittent fasting, or IF, you are missing out on a powerful – even revolutionary – everyday practice that can optimize your metabolic processes.
In its simplest version, IF requires 16 hours daily of not eating (the “fasting window”) followed by an 8-hour period of eating freely (the “feeding window”). This is called the 16:8 method. Other variations of IF – based on the same principle of feeding and fasting windows — include the 20:4 method (Warrior Diet) and the 23:2 method (One Meal a Day or OMAD).
If you are like most Americans, then chances are good that your health teacher in high school instilled the alleged importance of 3 meals a day. However, this eating plan is simply not based on science. If you never allow your body to take a rest from digesting and distributing energy from food (metabolism), you are missing out on the benefits of regular fasting, which include balanced hormones (including higher HGH levels), lower systemic inflammation, and better metabolic health.
``You can manipulate your metabolism to a degree. It is often a small change that may help you.``
The Bottom Line on Optimizing Your Metabolic Health
With the lifestyle modifications above – including HGH replacement therapy if you have a deficiency – you can reverse the course of worsening metabolic health and recover your youthful energy, peak physical performance, and a turbocharged metabolism.