Hormones and Frequent Urination in Men: What Is The Connection?
Table of Contents
- How the Male Urinary System Works
- Common Urination Issues With Age
- What Causes Frequent Urination in Men?
- Hormones and the Urinary System in Men: What’s the Connection?
- How Hormone Health Can Be Related to Frequent Urination in Men
- Common Urination Problems in Men: Symptoms, Possible Causes, and Treatments
- Preventing Urinary System Disorders in Older Men Using Human Growth Hormone (HGH)
Disorders of the male urinary system, including most notably frequent urination, often develop over time as part of the aging process. Older men are particularly vulnerable to developing urinary system disorders.
While the causes can be numerous, hormones play an important role in these conditions. In turn, hormone replacement therapy (HRT) with human growth hormone (HGH) can help to reverse such disorders and restore normal urinary function in men who receive treatment.
Let’s get into all the details of various urinary system disorders, their symptoms, and, most importantly, how men can reclaim their health with HGH therapy and other interventions.
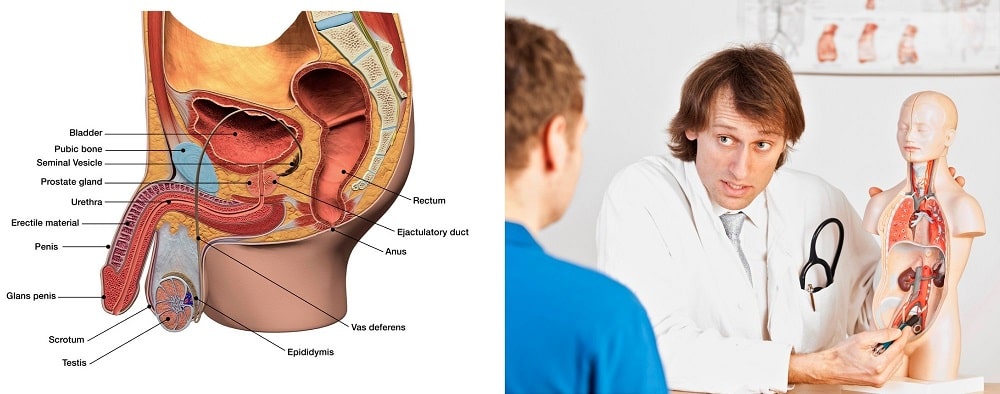
How the Male Urinary System Works
The male urinary system uses a complex method to remove waste and byproducts from diet and pass it through and out of the body. The key components of the male urinary system include:
- Kidneys. These organs remove drugs, waste products, urea from the blood, and other debris from the body and regulate the proper balance of electrolytes
- Ureters. These tubes act as a transport system, conveying the urine from the kidneys into the bladder
- Bladder. This triangular organ found in the lower abdomen acts as the storage unit for urine before it is pushed through the urethra for urination. The bladder can typically store about two cups of urine before emptying. However, some health conditions, as we will explore, can reduce this threshold.
- Sphincter muscles. These “rubber-band”-like muscles keep the urine from leaking out of the urethra for bladder control purposes. Over time, they may weaken, which could lead to bladder leakage. The sphincter muscles are divided into two types: internal sphincter muscles in the bladder neck that contract upon signal from the brain and external sphincter muscles that enclose the internal sphincter muscles to exert pressure and keep them tight.
- Prostate. This is a walnut-shaped gland that produces semen, and so is an important part of the male reproductive system. In addition to its role in male sexual health, the prostate surrounds the urethra at a critical juncture, the bladder neck. So, urine going through the urethra on its way out of the body must pass through the prostate.
- Urethra. This is the tube through which urine finally exits the body. The brain triggers the bladder muscles to tighten, which then forces urine to pass through the urethra and out of the body via the penis.
Urine contains a combination of the following materials that the body must pass regularly to maintain its normal function:
water
- inorganic salts
- urea (from amino acid metabolism)
- ammonia
- creatinine
- pigmented products of blood breakdown
- urochrome (which gives urine the typically yellowish color)
- electrolytes (including chloride, sodium, and potassium)
The makeup and appearance of a man’s urine can tell a lot about his current state of health.
What healthy urine looks like:
- Transparent
- Light yellow
- Pale straw
What unhealthy urine looks like:
- Honey-colored or dark urine (a sign of dehydration)
- Dark brown urine (a sign of a liver problem and/or extreme dehydration)
- Red or pink-tinted urine (a sign of blood; follow up with a specialist doctor is required)
Common Urination Issues With Age
A large percentage of men experience urination issues that appear over time. In fact, age-related urination problems are some of the most common conditions that affect older men.
In practical terms, urination issues can cause the following effects:
- Frequent urination during nighttime (you may have to get up several times throughout the night which can negatively impact your ability to get high-quality sleep, potentially leading to other health issues)
- Urinating more often throughout the day (more than once every few hours)
- Painful urination
- Urinary incontinence (you can’t hold it in)
- The urine stream begins slowly (you have to stand and wait for a while before things start moving)
- Urine dribbles after finishing
- The bladder still feels full after emptying
- Feeling like you need to go immediately or soon after going
The following conditions impacting the male urinary system may arise due to any number of factors, which can often work in combination with one another. The triggers of common urination problems in men, which are often interrelated, can include:
- Inflammation of the prostate gland (prostatitis). Chronic stress, nerve damage, or even bacterial or viral infection can cause the prostate gland to swell, which can impact the urethra.
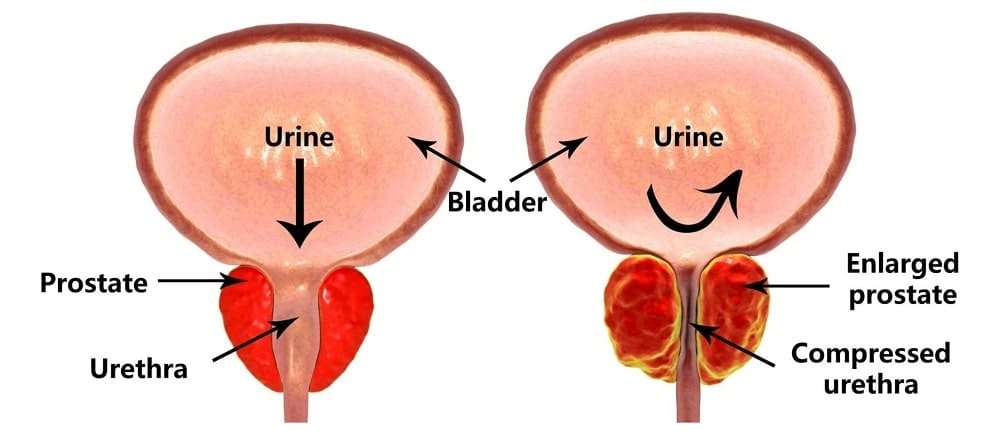
- Benign Prostatic Hyperplasia (BPA). The most common issue affecting the prostate in men over 50, BPA is characterized by a prostate that grows due to a combination of aggravating factors like exposure to environmental toxins such as bisphenol A (BPA), testosterone deficiency, and other factors.
- Bladder cancer. As the fifth-most common type of cancer in the United States, millions of men each year are impacted by bladder cancer. In addition to other symptoms, bladder cancer affects normal urination. Examples of common symptoms related to bladder cancer include blood in urine (haematuria), painful urination (dysuria), and frequent urge to urinate (urinary urgency)
- Inflammation of the urethra (urethritis). As opposed to many of the conditions discussed here which primarily affect older men, urethritis is more common in men between 20-35 years of age. It is often caused by pathogens like viruses and bacteria, usually due to sexually transmitted diseases (STDs).
- Urinary tract infection. Although more common in women, men can also experience urinary tract infections. Urinary symptoms due to such infections include cloudy urine, painful urination, foul-smelling urine, urinary urgency, and pain in the lower abdominal area.
- Hormone imbalances/hormone deficiencies*
*In an upcoming section, we’ll discuss the critical role that hormones play in the regulation of the urinary system in men, and what you can do about hormone-related urinary issues, including correcting the problem with hormone replacement therapy (HRT) using recombinant human growth hormone (rHGH).
What Causes Frequent Urination in Men?
Frequent urination can have a single or many causes, which may or may not be interconnected. Some of these causes are indicative of serious disease while others can be safely and effectively managed with lifestyle or dietary changes.
The causes of frequent urination in men include:
- Kidney or ureter problems
- Mental health conditions like generalized anxiety disorder (GAD) or others
- Diabetes insipidus
- Diabetes mellitus
- Prostate gland problems such as BPH or prostatitis
- Interstitial cystitis
- Diuretics (medications commonly used to treat high blood pressure)
- Hypercalcemia (too much calcium in the blood)
- Hyperthyroidism (overactive thyroid gland)
- Radiation therapy for cancer treatment
To diagnose the root cause of frequent urination, your medical provider will likely ask the following questions:
- Is your urine darker/lighter than normal?
- Are you consuming more or less water than usual?
- Do you have other symptoms not related to the urinary system?
- Does the issue occur at night, during the day, or both?
- How much alcohol and/or caffeine do you regularly consume?
- What, if any, medications are you currently taking?
Common medical tests to diagnose the cause of urinary symptoms in men that your doctor may order can include:
- Urinalysis.
- Blood Tests*.
- Cystometry (to measure the pressure inside of the bladder).
- Ultrasonography.
- Neurological Tests.
- Cystoscopy.
*These blood panels will likely include hormone screenings to measure testosterone, estrogen, human growth hormone (HGH), cortisol (the “stress hormone”), and/or other hormone levels.
Once diagnosed, your doctor will develop a customized treatment strategy, often multi-faceted, that can include:
- Kegel exercises to strengthen the muscles we discussed early responsible for controlling the urethra and bladder.
- Bladder retraining by forcing the bladder to go longer between each emptying.
- Diet modification to eliminate common foods that trigger bladder dysfunction like alcohol, caffeine, tomatoes, chocolates, spicy foods, and artificial sweeteners.
- Regulating fluid intake (enough to remain hydrated but not too much so as to trigger frequent urination).
- Medications to optimize urine flow.
- Surgery (usually reserved for extreme cases).
- Hormone replacement therapy (HRT).
Hormones and the Urinary System in Men: What’s the Connection?
Hormones, the signaling molecules or “chemical messengers” in the body, control the daily function of every major organ and system, including the urinary system.
Specifically, the hormones play a vital role in the development and health of the prostate gland, which undergoes two major growth phases:
- First, during puberty, the male sex hormone testosterone, along with human growth hormone (HGH), triggers the growth of the prostate gland to an average weight of 20 grams (.7 oz.)
- Second, the prostate begins to grow again around age 30, and continues to increase in size over time. By the time a man reaches 70 years of age, his prostate gland will weigh an average of 40 grams (1.4 oz.), an almost doubling in size.
This age-related second growth phase is why prostate issues typically affect older men.
The prostate gland is so important because it encompasses the urethra. So, if the prostate gland is too enlarged, not functioning properly, or otherwise compromised, it will have a downstream effect on urination.
The female sex hormone estrogen also plays a huge role in many men’s urinary system conditions, most notably BPH:
“Benign prostatic hyperplasia (BPH) and associated lower urinary tract symptoms (LUTS) are common clinical problems in urology and affect the majority of men at some time during their lives. The development of BPH/LUTS is associated with an increased ratio of estrogen to androgen levels, and this ratio, when mimicked in a variety of animals, induces BPH and lower urinary tract dysfunction (LUTD).”
The important thing to note here is that it is not only the raw estrogen count in men that matters, but also the ratio of estrogen to the androgen (male sex hormone) testosterone.
The bad news on this front is that men tend to lose, on average, roughly one percent of their total testosterone count each year following the all-time high in late adolescence.
Therefore, falling testosterone levels – and, by extension, falling ratios of testosterone to estrogen – are detrimental to men’s urinary health, in addition to causing a multitude of other symptoms like cognitive decline and muscle atrophy.
In addition to the sex hormone connection to urinary system disorders in men, human growth hormone, in combination with its partner molecule, insulin-like growth factor 1 (IGF-1) plays an important role in protecting the male urinary system.
Later on, we’ll cover the specific ways that HGH supports male urinary health.
How Hormone Health Can Be Related to Frequent Urination in Men
Noctura – a condition in which you awaken throughout the night to urinate – correlates to lower testosterone levels (hypogonadism) in men:
``Nocturia is significantly associated with testosterone deficiency, lower urinary tract symptoms (LUTS), and sleep disorders. The development of LUTS is commonly associated with testosterone deficiency in elderly men, and recent studies have suggested that testosterone has an ameliorative effect on nocturia. In hypogonadal men with nocturia, a negative feedback cycle can arise, in which testosterone deficiency leads to the development of nocturia, and nocturia contributes to the decline in testosterone levels.``
Hormone replacement therapy (HRT), the researchers note, can treat nocturia and other forms of frequent urination in men.
Common Urination Problems in Men: Symptoms, Possible Causes, and Treatments
Let’s cover some of the most common urination problems in men, their symptoms, possible causes, and treatments.
Painful Urination
Known clinically as dysuria, painful urination affects
Symptoms of painful urination in men:
- Painful urination. Pain during urination at the start might indicate a urinary tract infection, while pain after urination might indicate a bladder or prostate issue
- Burning
- Stinging
- Itching
- Abdominal pain
Possible causes of painful urination in men:
- Cancer
- Bladder or urethra inflammation (urethritis)
- Prostate disease
- Urinary tract infections, possibly including infections from outside of the urinary tract (potentially diverticulosis and diverticulitis)
- Sexually transmitted disease (STD)
- Side effects of medication
- Dehydration
- Hormone imbalances
Remedies for painful urination in men vary depending on the root causes and include:
- Adjusting medications
- Treatment of any current infections
- Increased hydration
- Treatment (pharmaceutical or surgical) of any underlying prostate or bladder disease
- Hormone replacement therapy (HRT)
Can painful urination in men be related in hormones?
Yes, hormonal imbalances, including testosterone and growth hormone deficiencies, can trigger prostate issues as well as systemic inflammation, both of which are common causes of painful urination.

Bladder/Urinary Tract Infection in Men
Occasionally, viruses, bacteria, or other pathogens can get into the bladder and/or urinary tract and cause a number of uncomfortable and sometimes dangerous symptoms. Clinicians refer to bladder infections in men as “cystitis.”
Symptoms of urinary tract/bladder infection in men:
- Blood in urine (hematuria)
- Trouble urinating (incomplete emptying)
- Frequent urination
- Low-grade fever
- Urgent need to urinate (urgency)
- Cloudy, discolored urine (often accompanied by a strong odor)
- Burning/tingling sensation during/after urination (dysuria)
Possible causes of urinary tract/bladder infection in men:
- Recent urinary tract surgery
- Fecal incontinence
- Immobility
- Being uncircumcised
- Being immobile for long periods
- Not drinking enough fluids
- Untreated diabetes
- Engaging in anal intercourse (due to a greater exposes to bacteria such as Escherichia coli, or E. coli)
In addition to the potential triggers of urinary tract/bladder infection above, the following conditions put men at increased risk of developing them:
- Enlarged prostate (benign prostatic hyperplasia aka BPH)
- Kidney stones
- Abnormally narrowed urethra (urethral stricture)
- Recent use of urinary catheter (a tube to drain your bladder)
- Some surgical procedures that require opening the urethra
Remedies for urinary tract/bladder infection in men:
- Antibiotics/antivirals
- Lots of water (hydration)
Can urine infection in men be related to hormones?
Possibly. Hormones like testosterone and human growth hormone (HGH) enhance immune system function. Conversely, a deficiency of these hormones can negatively impact the body’s ability to fight off infections, including of the bladder or urinary tract.
Weak Urine Stream in Men
Weak urine stream is a common ailment affecting primarily older men, and most often indicates a dysfunctional prostate and/or urinary tract.
Symptoms of weak urine stream in men:
- Inability to completely empty
- Sense of urgent need to go (often soon after urinating)
- Cloudy urine
- Dribbling
Possible causes of weak urine stream in men:
- Nervous system disorders or problems with the spinal cord
- Dysfunctional prostate or urinary tract
- Certain medications (including antidepressants, remedies for colds, and drugs used for incontinence)
- Surgery side effects
- Scar tissue (stricture) in the urethra
- Spastic pelvic muscles
Remedies for weak urine stream in men:
- Medication to treat enlarged prostate
- Surgery to relieve a prostate blockage (transurethral resection of the prostate, TURP)
- Antibiotics to treat an infection
- Surgical intervention to dilate/cut scar tissue located within the urethra
- Hormone replacement therapy (HRT)
Can weak urine stream in men be related to hormones?
Yes. Weak urine stream is strongly correlated in most instances with prostate dysfunction, which in turn is often linked to hormone deficiencies, especially in older men.
Blood in Men’s Urine
Blood in the urine (hematuria) is a potentially serious medical condition that requires immediate care from a professional medical provider. Men who notice any trace of blood in the urine, including pink tint to the urine, should seek help right away.
Symptoms of blood in men’s urine:
- pink, brown, or red urine
Possible causes of blood in men’s urine:
- Prostate problems
- Urinary tract infections
- Kidney stones
The following factors might put men at greater risk of hematuria:
- Age over 50
- Family history of urinary bleeding
- Overtraining
- Recent kidney infection
- Some medications like nonsteroidal anti-inflammatory pain relievers, aspirin, and antibiotics
Remedies for blood in men’s urine:
- Prescription medication
- Shockwave therapy (for kidney stones)
Can blood in men’s urine be related to hormones?
Usually blood in men’s urine has another cause, but in cases where the underlying cause is an enlarged prostate, human growth hormone (HGH) replacement therapy can be a powerful treatment tool.
Preventing Urinary System Disorders in Older Men Using Human Growth Hormone (HGH)
As we mentioned previously, maintaining optimal human growth hormone (HGH) levels across time is critical for anti-aging care, including for protecting men’s urinary function. HGH supports male urinary health in key ways:
- Normalizes blood sugar/insulin sensitivity which, in turn, can prevent and treat diabetes (a leading cause of urinary health issues in men, as we discussed earlier)
- Prevents the development of various autoimmune diseases that can impact the male urinary system, including autoimmune diabetes
- Reduces systemic inflammation which contributes to urinary system disorders, including inflammation of the prostate (prostatitis)
- Reduces the “stress hormone” cortisol which is often the culprit of frequent urination and other types of bladder dysfunction
- Increases testosterone secretion by the gonads which supports normal prostate function
HGH is safe for patients in terms of protecting urinary system function. Recent research has confirmed that HGH produces no increase in serum prostate-specific antigen (PSA) in treated men and therefore does not contribute to cancer growth, as some have speculated in the past.
Because HGH levels tend to drop as men age, if you are over 40, it is very likely that you have an HGH deficiency (called “growth hormone deficiency” or GHD in clinical settings) that is impacting your urinary system health.
Falling HGH levels also result in lower IGF-1 levels, creating further hormonal imbalance and contributing to greater declines in urinary system health in men.
That’s why getting tested is essential for men over 40 experiencing any of the signs or symptoms of urinary dysfunction that we’ve described here, including painful urination, weak urine stream, frequent urination, etc.
A simple blood test can determine if a man is experiencing clinical growth hormone deficiency. In cases where tests confirm the presence of a disorder, hormone replacement therapy (HRT) with recombinant human growth hormone (rHGH) in the form of somatropin safely and effectively increases circulating HGH levels for optimal urinary system health.
Norditropin
Genotropin
Price: starts from $ 420
Category: HGH Injections
Manufacturer: Pfizer
Options: 0.2, 04., 0.6, 0.8, 1.0 mg